Abstract
Introduction
Primary Plasma Cell Leukaemia (pPCL) is a rare disorder and considered the most aggressive plasma cell dyscrasia. Autologous stem cell transplantation (auto) has been shown to improve outcomes, however the role of allogeneic transplantation (allo) is uncertain. The CIBMTR compared outcomes of 147 patients undergoing auto and allo transplant and demonstrated that while allo patients had significantly lower relapse rates their non-relapse mortality was significantly higher. Further evidence is needed to guide clinicians in choosing between auto versus allo in transplant eligible patients.
This study examines the largest cohort of patients with pPCL undergoing auto and allo transplantation.
Materials and Methods
A retrospective analysis was undertaken of the European Group for Bone Marrow Transplantation (EBMT) experience of patients with pPCL undergoing transplantation between 1998 and 2014. Only patients who had achieved Complete Response (CR), Partial Response (PR) or Stable Disease (SD) prior to transplantation were included.
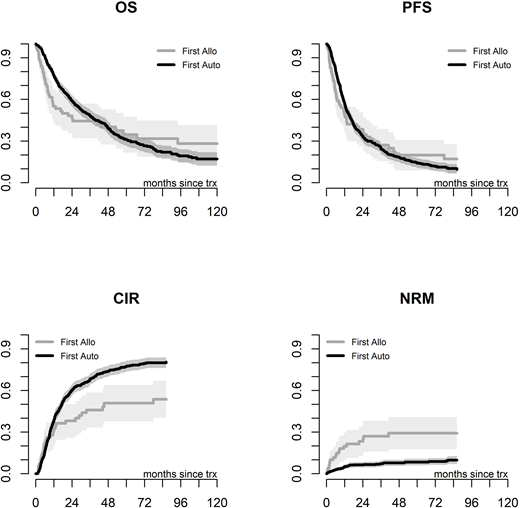
The primary end point was Overall Survival (OS). We further analysed Progression-Free Survival (PFS), Cumulative Incidence of Relapse (CIR) and Non-Relapse Mortality (NRM).
As this is a retrospective study single- and tandem- transplant groups were compared by landmark analysis (4 months post first auto) and dynamic prediction to avoid time bias. We defined tandem transplants (auto-auto or auto-allo) given within 9 months in absence of progression. Dynamic prediction was used to predict long-term outcomes in all patients according to the treatment actually received and without loss of information as in the traditional landmark analysis.
Results
A total of 751 patients were included in the analysis. 70 patients received an allo as first transplant. 681 patients received an auto as first transplant; 239 of these patients went on to receive an elective tandem transplant. 122 had a tandem allo and 117 had a tandem auto.
Patients having first allo were younger (median age 47.2 years versus 57.7 years for first auto), had a longer time from diagnosis to transplant (first allo 84.3% transplanted in <12 months versus 93.5% in first auto) and had higher proportion of patients both in CR and SD (CR allo 37.1% versus 32.5% first auto, SD 15.7% allo versus 4.8% in first auto). For patients receiving a tandem allo there was a higher proportion of matched unrelated donor transplants (50% versus 28.6% in first allo) and reduced intensity conditioning (80.3% versus 27.1% in first allo).
The median OS was 17.5 months for first allo versus 33.5 months for first auto, while median PFS was 11.7 months for first allo and 14.3 months for first auto. As demonstrated by Figure 1 the OS and PFS curves do cross, therefore LogRank test was not appropriate. At 36 months NRM was 27% for allo versus 7.3% for first auto (p<0.0001) which likely accounts for the differences in OS.
Figure 1. OS, PFS, CIR and NRM
Landmark analysis at 4 months resulted in a reduction in the number of second transplants analysed to 160 patients. The landmark analysis revealed that there is no significant difference in OS or PFS between the transplant groups, and lower CIR (p=0.07) and only a limited early increase of NRM (p=0.24) in the auto-allo group. These results were substantially confirmed when adjusting for covariates, however the landmark analysis is limited by reduced sample size and non-constant relative risks.
Dynamic prediction was made with a horizon time of 3 years for OS and 1 year for PFS. Age and disease status at transplant were included and all transplant strategies were compared to single auto as baseline. This revealed that tandem auto allo had a significant improvement in 1 year PFS with a 44% reduction in risk compared to single auto (HR 0.56, p=0.003). The 3 year predicted OS reveals a trend towards superiority for tandem auto allo versus single auto but it did not reach significance (HR 0.78, p=0.20).
Conclusion
This is largest retrospective study examining transplantation in pPCL.
Direct comparison of first allo versus first auto shows that in the short term allo upfront has worse outcome, largely due to significant NRM. Landmark analysis and especially dynamic prediction models reveal for the first time that auto-allo has an acceptable NRM and could be preferred to single auto due to lower relapse rates translating into a better PFS and even a trend for OS in the long term.
Lawless:Celegene: Honoraria, Speakers Bureau; Abbvie: Membership on an entity's Board of Directors or advisory committees. Foà:AMGEN: Other: ADVISORY BOARD; INCYTE: Other: ADVISORY BOARD; ABBVIE: Other: ADVISORY BOARD, Speakers Bureau; JANSSEN: Other: ADVISORY BOARD, Speakers Bureau; GILEAD: Speakers Bureau; ROCHE: Other: ADVISORY BOARD, Speakers Bureau; CELTRION: Other: ADVISORY BOARD; CELGENE: Other: ADVISORY BOARD, Speakers Bureau; NOVARTIS: Speakers Bureau. Garderet:Takeda: Consultancy; Amgen: Consultancy; Celgene: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal